Overreaching is a term used to describe an acute training phase during which you temporarily increase the training volume, load, and/or intensity as part a specific training strategy to gain a specific training outcome. When properly programmed, overreaching can be an effective and important part of a training cycle. Unlike Overtraining Syndrome (OTS), overreaching is an actual training strategy to build strength and/or performance. Although it typically results in additional fatigue and soreness, you can easily recover with a few days of rest and a specific recovery plan. After resting, the desired outcome is an obvious improvement or supercompensation in that specific sport or activity.
Overreaching is an important component of high-quality training. When utilizing overreaching, please be aware of the potential to develop Overtraining Syndrome (OTS). Please refer to 12 Tips to Prevent Overtraining Syndrome for the warning signs. Overreaching is an advanced training concept and shouldn’t be utilized by novice individuals regardless of the sport or activity.
Why risk Overtraining Syndrome to incorporate overreaching into your training?
- Overreaching helps your body to perform the extra steps needed to produce more results in a shorter period of time.
- Overreaching helps you “shock” the body in order to improve. During a short period of time (days to weeks), you push yourself to a state of being nearly overtrained prior to backing off. This is more than the typical overload you are attempting with regular training.
- Supercompensation occurs as you push yourself to the limit. Then you pull back from the brink of being overtrained as you transition into a rest and recovery phase, which is outlined in 12 Tips to Prevent Overtraining Syndrome and 10 Tips to Self-Treat Overtraining Syndrome.
- Quality intermediate to advanced training plans incorporate a stair step increase in performance with 3-4 intermittent bouts of overreaching throughout a typical periodized training year. Make sure that your training plan is right for you.
6 tips on how to safely overreach to advance your training:
- A planned and programmed overreaching session should last no longer than 1-2 weeks.
- Increase your training, intensity, and/or volume no more than 40%. For example, if you typically run 50 miles a week, then plan on a week or two of 70 miles before your scheduled rest and recovery days. You may also choose to combine two harder variables in one training session. Combine a long run with challenging hills, a tempo session with speed work, or take a long run after performing a high intensity interval training session (HIIT).
- Watch for the following warning signs of overtraining syndrome: feeling fatigued sooner during the workout; excessive fatigue or soreness; changes in appetite (larger or smaller); and a longer post workout recovery time. If you’re experiencing these symptoms, then you are into overreaching and on the verge of overtraining. Depending on how much longer in the phase you need to progress, you may need to discontinue your overreaching training plan and initiate your recovery protocol.
- During the overreaching cycle, be sure to properly recover between each bout of exercise. Implement specific recovery strategies including: extra sleep; adequate nutrition and hydration; proper supplementation; and foam rolling.
- Plan a 5-7 day recovery protocol. Several methods to help you to recover are outlined in outlined in 12 Tips to Prevent Overtraining Syndrome and 10 Tips to Self-Treat Overtraining Syndrome. Find more recovery tips in Muscle Cramping & Spasms – Treatment Options.
- Once you complete your recovery time, continue with your training plan. Take note of where you are and how you feel in your training. If you are feeling well and are demonstrating improvement, be sure to adjust your training plan by appropriately tapering up the volume and/or intensity to match your added gain. For example, if you were squatting 200 lbs. as a part of your work sets, you may increase the weight by 5-10% for a total of 210 or 220 lbs. This would also be the case for any other exercise or running distance and/or pace.
Overreaching can be an excellent method to speed up and quickly advance in your training. Overreaching increases your risk of developing Overtraining Syndrome (OTS). It should be performed carefully and thoughtfully as part of a complete training plan. Overreaching should always be followed with an equally thought out rest and recovery protocol. During your overreaching cycle, document your training and recovery strategies so that you can refine your process. It will make your next attempt at overreaching even more effective and safe in the future.
Discover how you can continue to train hard and avoid the associated poor performance, illness, and injury that can result in lost training days and opportunity!
AVAILABLE NOW ON AMAZON!
In my book, Preventing and Treating Overtraining Syndrome, I show you how to recognize the risk factors and symptoms of OTS. You’ll learn how to utilize prevention strategies to help you develop a personal training strategy that will allow you to push past your limits and prior plateau points in order to reach a state of what is known as overreaching (your body’s ability to “supercompensate”). This will speed up your results, so that you can train harder and more effectively than ever before! In addition, learn how to use the foam roller (complete with photos and detailed exercise descriptions) as part of a health optimization program, recovery program, rest day or treatment modality.









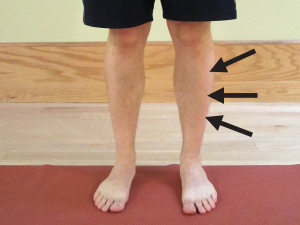
In this guest post for Marathon Training Academy, you will discover the risk factors for plantar fasciitis and learn how to quickly return to your running routine with these self-treatment techniques!