Q. I have been diagnosed with a T-6 spinous process fracture. I have been prescribed a thoracolumbar brace for 12 weeks. If it takes away the pain, I’m willing to try it. What do you think generally of braces? I like swimming, walking, Pilates, and yoga. All of that is out right now except the walking. I have osteoporosis and compression fractures at T-6/7 and T-11/12. I would love your insight on healing time or ability to get back to the activities I love. I was encouraged to read the Q & A on the teenager who had the C-7 spinous process fracture, but my story is quite a bit different. Thank you! -Mary
(Please note that the original question was much more detailed and personal, so it was truncated. The name has been changed for privacy.)
A. Thanks for the great question! For general discussion purposes, I will address the following topics: bracing; healing and recovery times; osteoporosis; and treatment.
Bracing
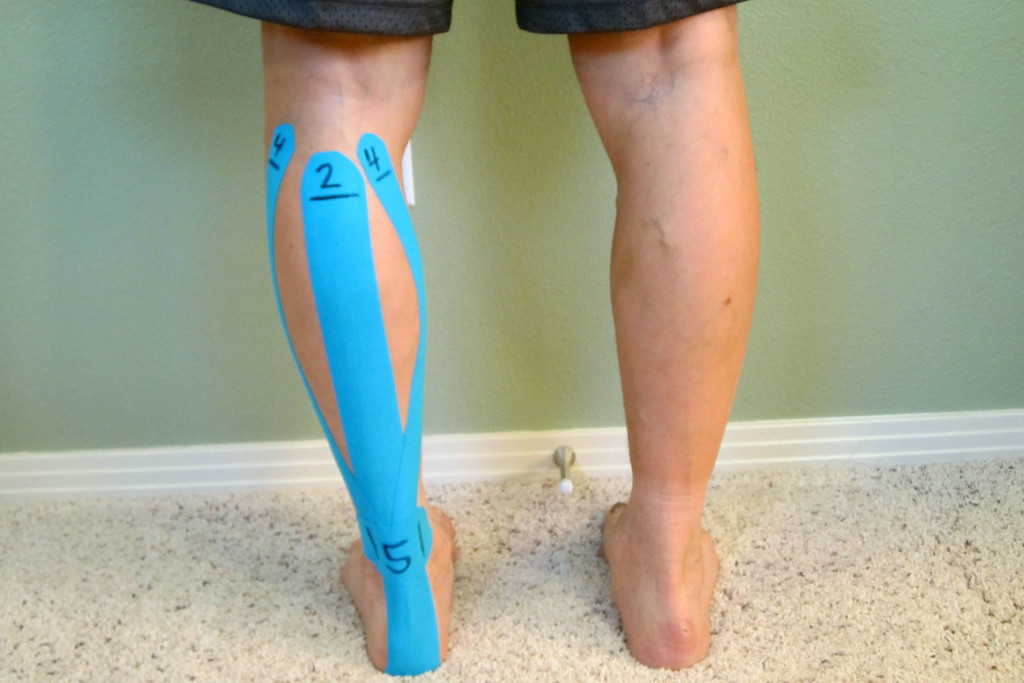
Lumbar and thoracic braces can be appropriate and necessary tools for the right circumstances. Corset style braces and/or more rigid style bracing are typically prescribed for either of the following two reasons: to stabilize an injury site that the physician is concerned that movement may compromise healing or safety or to stabilize an area in the hope of reducing pain. In this particular case, a brace was likely prescribed for both reasons.

There are many potential down sides to wearing a brace. It can be uncomfortable and inconvenient to wear. More concerning, bracing can lead to over dependence and the loss of important muscle stabilization strength. This is why an appropriate exercise program should be maintained while wearing the brace. Once you’re cleared to wean from the brace and taper back into normal activities, you can progress into a more targeted and comprehensive exercise plan.
Healing and Recovery Times
Whether or not a spinous process will heal depends on the severity of the fracture. Is it a small fracture with the bones still attached (basically a crack) or was the spinous process separated from the vertebrae? If the two pieces were separated, then it is likely they will not heal back like a normal fracture. The bone will not re-attach itself back to vertebrae. When this occurs, it’s known as a non-union. Scar tissue and fascia will surround the injury site and in most cases, form a solid fibrous pseudo-union between the two pieces of bone.
In most cases, there aren’t any deleterious effects from the injury and healing process. Like bone healing, this process typically takes 6 to 8 weeks for most individuals. It can take longer based on other factors: age; nutritional status; smoking; and other conditions such as osteoporosis or diabetes. Even certain medications, such as NSAIDs, may impede bone healing. Speak to your physician and pharmacist about any and all medications and supplements you are taking.
(In Mary’s particular case, there may be other compounding factors or the fractures were quite severe since the expected time frame for healing is 12 weeks.)
Compression fractures will likely take about the same amount of time to heal. If the bone is slightly collapsed, it will not recover its previous shape. It will remain slightly more wedge shaped.
Osteoporosis
Although bracing is often a necessary part of the recovery, it will likely weaken the surrounding musculature. A strong core and adequate stability of the muscle around the trunk are important components to one’s recovery as well as prevention for ongoing issues (particularly in cases of compression fractures).
Be proactive in dealing with your osteoporosis. Otherwise, you will likely continue to experience fractures and other issues. There are medications that can help, but they all have significant potential risks.
Proper nutrition and weight training are components to managing osteoporosis. Please refer to Why Astronauts Resistance Train and So Should You.
In addition, I recommend Sara Meeks’ book, Walk Tall! An Exercise Program for the Prevention & Treatment of Back Pain, Osteoporosis and the Postural Changes of Aging.
Treatment
Nutrition is very important for healing. Consult with a functional medicine practitioner to dial in your nutrition and address any potential nutrient deficits or nutrient absorption issues. Also, refer to Why You Won’t Heal – Poor Nutrition.
I recommend starting with a walking program that includes a gradual taper up to at least 3 miles per day. Once you’re medically cleared to exercise again, find a physical therapist (PT) that specializes in osteoporosis management. The American Physical Therapy Association (APTA) offers a wonderful resource to help find a physical therapist in your area.
A PT can help you initiate a comprehensive core stabilization program along with weight training. In many cases, a core stabilization program can be initiated around the 6 to 8 week mark, but it depends on when your physician clears you to return to exercise other than walking.
Prior to initiating a full strength training routine, begin by initially focusing on your back extension strength (which will address the spinous process fractures as well as the compression fractures). Any rehabilitation program should be slow and steady. Start well before the 12 week period unless there are medical contraindications for doing so based on your particular situation.
Healing times vary tremendously. It’s based on the severity of the injuries and your individual health status. With poor bone health or other co-morbidities, it could be prolonged. Full healing may take 4 months or so.
With these types of injuries, pain is always highly variable. It can vary from a couple of weeks to 4-6 months. Pain will typically slowly decline as the healing process progresses. The early inflammatory process that was initiated after the injury will progress through an acute to more subacute phase. Wearing the brace usually helps with early pain management.
Thankfully, this type of injury usually results in a full return to function without many long-term deleterious effects. The key is to allow adequate healing time, and then slowly and strategically progress back into full activity.
Have you ever suffered from a thoracic spinous process fracture? Please share your story below.
If you have a question that you would like featured in an upcoming blog post, please comment below or submit your question to contact@thePhysicalTherapyAdvisor.com. Be sure to join our growing community on Facebook by liking The Physical Therapy Advisor!
Disclaimer: The Physical Therapy Advisor blog is for general informational purposes only and does not constitute the practice of medicine or other professional health care services, including the giving of medical advice. No health care provider/patient relationship is formed. The use of information on this blog or materials linked from this blog is at your own risk. The content of this blog is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Do not disregard, or delay in obtaining, medical advice for any medical condition you may have. Please seek the assistance of your health care professionals for any such conditions.