Q. My son was recently injured in a weight room accident that resulted in a C7 spinous process fracture. The neurosurgeon says not to worry about it and that he can return to sport in six weeks. He is a very talented athlete, and he’s trying to get a college football scholarship. I’m concerned for his safety and scholarship prospects. Do you have any advice? -Jennifer
A. I am so sorry to hear about your son’s injury, Jennifer. Weight lifting is such a critical component to any training program as well as for those who are trying to maintain muscle mass and general health. Sadly, accidents happen and can be very serious. However, weight training will be an ongoing critical training component if your son is to compete in football at a collegiate level.
Thank you for letting me share his imaging pictures. Viewing the imaging allows for a better discussion, but please note that I have not evaluated your son. The following advice is only for the purpose of general discussion.
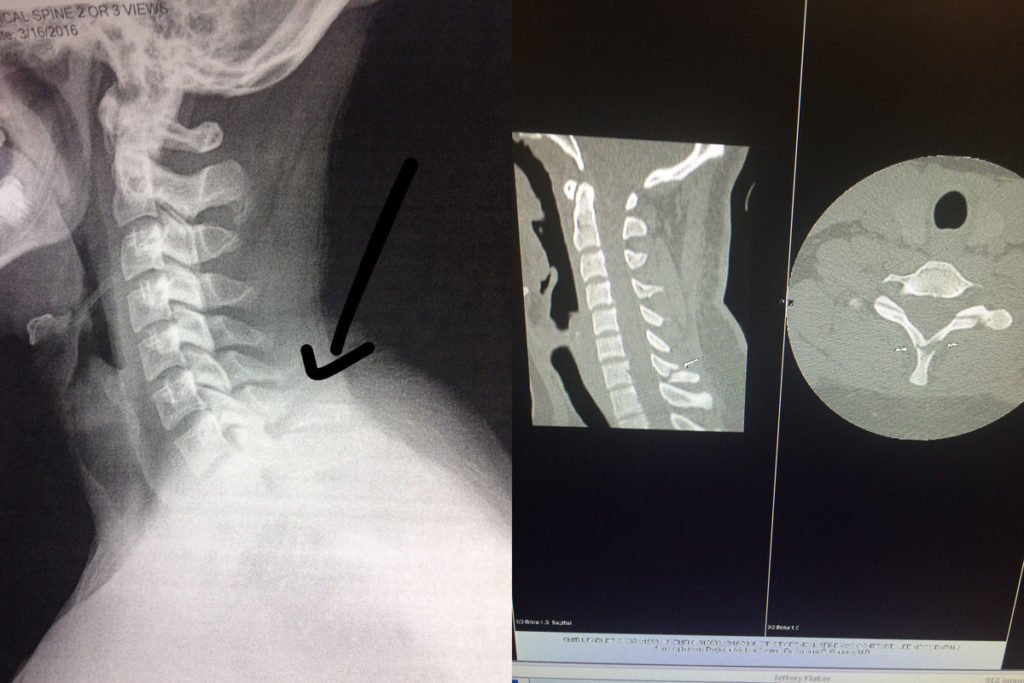
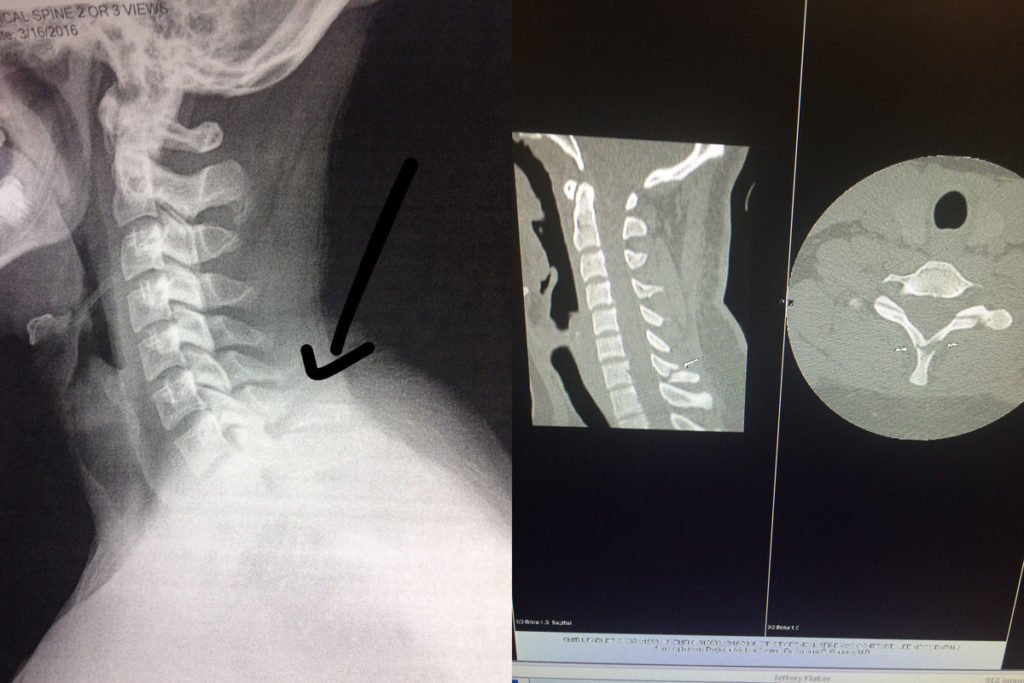
(Left: X-ray of C7 fracture. Right: CT Scan of C7 fracture.)
As you can notice on the imaging provided, only the spinous process was injured. Although close to the lamina of the vertebra (which has a primary role of protecting the spinal cord), it was not injured. This was confirmed by the physician’s physical exam, X-rays, and CT Scan. I’m glad that the injury was taken seriously with appropriate medical follow up. One should never take unwarranted risks when evaluating spinal injuries.
This particular fracture is also known as a Clay Shoveler’s Fracture. This occurs when the end of the spinous process is either broken off by a physical impact (as in the case of Jennifer’s son when the barbell hit his neck) OR as a result of the muscle pulling so hard that it breaks the bone and literally tears off part of the spinous process. The role of the spinous process, particularly in the cervical region, is to help limit cervical hyper extension. More importantly, the spinous processes are there as an attachment point for muscles and ligaments.
C7 is the largest cervical vertebrae in the neck. The C7 vertebra is right in the middle of transition from the cervical spine to the thoracic spine and is home to many fascial attachments and muscular attachments from the neck and shoulder girdle. Many of the deeper neck extensors and rotators such as the splenius capitus and splenius cervicis as well as the trapezius, rhomboids and serratus posterior muscles have C7 attachment points.
Typical Symptoms
In most cases, there is pain immediately after the injury which is often described as a burning or “knife-like” stabbing pain. Other symptoms include muscle tightness and sharp pain that increases with repeated activity and movement of the neck or shoulder girdle. The pain is often described as feeling similar to a severe muscle strain in the upper back. The area of fracture as well as the nearby spinous processes is typically very tender as are the nearby muscles.
If only the spinous process is injured, you should not see any neurologic symptoms. You will likely see loss of cervical motion and possibly shoulder motion as those motions will cause muscles to pull directly on the site of injury which limits one’s desire to move. Symptoms are typically worse with the head down or when the arms are active in front of the body (such as driving or working at the computer).
Treatment Considerations
Bone healing is a complex process and will differ significantly among individuals. Factors affecting bone healing include: the type of fracture and the patient’s age; underlying medical conditions; and nutritional status. For a person with good health status, the bone will take on average six to eight weeks to heal to a significant degree. In general, children’s bones heal faster than those of adults.
However, with a spinous process fracture that is separated to this degree, the bone will most likely never heal. The bone will not re-attach itself back to vertebrae. When this occurs, it’s known as a non-union. Scar tissue and fascia will surround the injury site and in most cases, form a solid fibrous pseudo-union between the two pieces of bone. In most cases, there will be no deleterious effects from the injury and healing process. Like bone healing, this process typically takes six to eight weeks for most individuals.
Acutely there is likely to be pain, but long-term pain typically subsides. However, as with all injuries, there is the risk of chronic pain or long-term irritation to the area associated with the muscle and tendon that insert/attach onto the spinous process involved in the injury.
Pain Management
Initially, I don’t recommend treating with NSAIDS (non-steroidal anti-inflammatory medication) as there is research that indicates that the healing response could be delayed. Instead and whenever possible, I would recommend other alternatives for pain management like applying heat or ice. Typically no more than 20 minutes per hour would be recommended, and don’t apply heat or ice directly to the skin (use a towel as a barrier).
Pain medication, such as acetaminophen, is always an option if recommended by your physician. You may also want to consider utilizing topical agents, which can help to decrease pain and muscle spasms. The method of action varies greatly according to the product used. You may find that one product works better than another. Some of my favorite products in my medicine cabinet include: Biofreeze Pain Relieving Gel; Arnica Rub (Arnica Montana, an herbal rub); and topical magnesium.
Another option is oral magnesium. You can take Mag Glycinate in pill form or by eating foods higher in magnesium such as spinach, artichokes, and dates. Taking additional magnesium (particularly at night) can help to reduce muscle cramps and spasming. It is also very helpful in reducing overall muscle soreness and aiding in a better night’s rest. Most people are deficient in the amount of magnesium they consume on a regular basis. I recommend beginning with a dose of 200 mg (before bedtime) and increasing the dose as needed. I would caution you that taking too much magnesium can lead to diarrhea. Mag Glycinate in its oral form is the most highly absorbable. Although not as absorbable, Thorne Research Magnesium Citrate and magnesium oxide can also be beneficial.
Soft tissue massage of the adjacent muscles as well as electrical stimulation can both be used to reduce pain. If pain persists, please discuss the options with your physician.
Activity Modification and Exercise Considerations
Activity involving the head, neck, and shoulders should be limited initially. In some cases, the physician may ask that a cervical collar be worn for several weeks. Opinions on this vary greatly and will be dependent on the exact location of the fracture.
The basic idea is to avoid heavy use of the muscles that would specifically pull on the injury site. This would include muscles that flex, extend, rotate or side bend the head as well any arm movements that move the shoulder. This would obviously include any type of heavy lifting or placing anything on top of the injury site like a barbell.
Although this seems very limiting, you can still move the neck and shoulders. Gently perform range of motion (ROM) of the neck and shoulders to maintain full mobility. This will also help to limit pain and muscle spasms of the surrounding tissues. The idea is to limit extreme movement, limit the movement under load, and limit the speed of movement.
I would specifically limit most activity for at least six to eight weeks to insure an adequate amount of scarring has occurred. In addition to the above noted limitations, I also wouldn’t perform any activities that would be jarring to the body (such as jogging). If you want to maintain your cardiovascular endurance, you could peddle on a stationary bike while keeping your upper body mostly relaxed.
At around the four to six week mark, I would slowly start working on the cervical extensor and shoulder girdle muscle exercises (as demonstrated below). You will want to engage the muscles symmetrically as to not cause asymmetrical pulling over the injury site. These exercises will help to engage the muscles (the cervical extensors and scapular muscles, including the rhomboids and trapezius muscle) specifically used to stabilize the injury site.

Begin by performing these I’s, T’s, and Y’s exercises on a Thera-Band Exercise Ball. Start slowly without resistance. Keep your chin tucked and head aligned with the body. Move your arms slowly up and down in each position of I, T, and Y. Start with 10 repetitions for 3 second holds, and then progress the number of repetitions as long as there is no pain.
Once you can easily and pain free perform 20 repetitions with 3 second holds, add a 1-2 pound weight in each hand and start the progression initially at 10 repetitions. Be sure to always let pain guide the progression. The exercise should remain pain free.
After the six to eight week mark, initiate a slow, but steady return to exercise. Start with lower extremity exercises such as the leg press, body weight lunges, squats or step ups. During this time, progress with targeted exercises designed to strengthen the muscles of the mid trapezius, rhomboids, and neck extensors.
Let pain guide your progression. If you perform an activity that causes pain near the injury site, then that activity should continue to be avoided in the short-term. Continue to perform exercises bilaterally to be sure that the force/pull over the injury site is symmetrical. For example, when you start on rowing, then it should be a two-handed row and not a one-handed version.
Progression of exercise of the associated muscles should be slow and again, pain should be carefully monitored. Any pain provoking movements early in the rehabilitation phase should be avoided. When returning back to weight training, start with a weight approximately 50% of your prior max. Work within that weight for a week or two, and then slowly progress back to the prior weight used (depending on your symptoms).
You may also return to light jogging. If there is no increase in your pain level, then slowly progress back into full running and sprinting.
Exercises to avoid for at least twelve weeks include: barbell squats; overhead press; power cleans; squat cleans; and snatches. Avoid anything that would put direct pressure over the injury site or exercises that include a speed and power component under load (such as the power clean).
Rehabilitation Recap
Due to the amount of information presented, I want to re-iterate the important parts of the rehabilitation process. Be sure that you have your physician’s clearance prior to resuming activity.
0-4 weeks: This is the time for pain management and activity modification. You want the area to scar down. Exercise and activity should be limited although you should maintain full range of motion (ROM) of the neck and shoulder girdle if possible.
4-6 weeks: Initiate a cervical stabilization program and scapulothoracic exercises starting without any resistance. Perform the I’s, T’s, and Y’s exercises on an exercise ball (as demonstrated above). Progress with these exercises and continue with cardiovascular exercise such as riding a stationary bike. You may also start bench pressing, but begin light and monitor your pain level.
6-8 weeks: Progress with shoulder and upper back exercises. Be sure to use two-handed movements. Depending on your pain level and strength, lower body exercises can be initiated. Begin with body weight exercises, and then progress to resistive exercises. Continue to limit direct pressure over the injury site or asymmetric forces. Lower body exercises, such as the leg press and dead lift, may be started. Exercise should be mostly pain free. If you experience pain during an exercise or movement, discontinue for now and then retry it in a week or two.
8-12 weeks: During this phase, slowly start tapering up on all activity. During this time, you can progress your jogging to eventually sprinting as well as road bicycling. You can progress back into lower extremity exercises as tolerated as long as there isn’t any significant associated pain at the injury site. Focus on neck and upper extremities exercises with two-hands/arms bilateral exercises. Focus on exercises that develop strength in the muscles surrounding the injury site without causing increased pain or asymmetrical force. The preference is for two-arm movements for now. This is also the time to start working on thoracic mobility to insure the entire vertebral chain can move freely. Be sure to have full shoulder and cervical mobility. Continue to avoid any specific pressure on the injury site. If you haven’t already, you could start the following: dead lifting; front squat; and lunges with load.
12+ weeks: Return to full activity. However, let pain and common sense continue to be your primary guide. At this stage, you can return to light squatting. I recommend a low-bar position as this typically lines up just below the spine of the scapula and should be below the C7 injury site. Start single arm movements, such as a one-armed row, as well as power movements, such as the clean and snatch. You can also initiate overhead lifting. The key is to progress slowly and see how your body responds. Begin with 50% of the load used prior to your injury.
If you don’t already own a copy, I would highly recommend that you purchase Starting Strength: Basic Barbell Training by Mark Rippetoe. This text should be regarded as the authority on strength training and should be used as a guide for beginners to advanced weight training enthusiasts.
Once a full return to weight training activities has been accomplished, a full return to sport should also be possible. Any sports that involve high impact, such as football or mixed martial arts, should have your physician’s approval in order to insure that the fracture is stable. In most cases, the level of pain present will be a great indication of how stable the injury site is.
If you are unsure about how to properly progress in your training and rehabilitation, I recommend that you work with a highly qualified trainer or sports medicine professional to insure that you are performing your particular exercise and sport in a manner that will keep you safe and the fracture stable. The American Physical Therapy Association (APTA) offers a wonderful resource to help find a physical therapist in your area. In most states, you can seek physical therapy advice without a medical doctor’s referral (although it’s a good idea to hear your physician’s opinion as well).
Good luck to your son and you, Jennifer! I hope you find this information helpful. Thankfully, this type of injury usually results in a full return to function without many long-term deleterious effects. The key is to allow adequate healing time, and then slowly and strategically progress back into full activity.
Have you ever suffered from a spinal fracture or avulsion fracture? Have you experienced an accident while weight training? Please share your story below.
If you have a question that you would like featured in an upcoming blog post, please email contact@thephysicaltherapyadvisor.com. For additional health and lifestyle information, join our growing community on Facebook by liking The Physical Therapy Advisor!
Disclaimer: The Physical Therapy Advisor blog is for general informational purposes only and does not constitute the practice of medicine or other professional health care services, including the giving of medical advice. No health care provider/patient relationship is formed. The use of information on this blog or materials linked from this blog is at your own risk. The content of this blog is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Do not disregard, or delay in obtaining, medical advice for any medical condition you may have. Please seek the assistance of your health care professionals for any such conditions.