Overtraining Syndrome (OTS) can affect any athlete in any sport or at any level. I have treated high school athletes to weekend warriors for OTS. Recently I have noticed more cases of OTS among CrossFit enthusiasts and runners of all distances. People are training harder and longer than ever before with wonderful results. At times, even the best of intentions can lead to not so desirable consequences. OTS usually starts with muscle soreness and a feeling of fatigue. Then it quickly progresses into a case of overtraining syndrome or injury. Overtraining can occur when the intensity and/or volume of exercise becomes too much for the body to properly recover from. For my tips and strategies to prevent OTS, please refer to 12 Tips to Prevent Overtraining Syndrome. In this follow up post, I will specifically address how to self-treat OTS.
Overtraining Syndrome will significantly impede your performance and frequently leads to a serious injury. In OTS, your body isn’t able to adequately handle or adapt to the high volume and intensity of exercise that you are performing. If you develop OTS, you will need to take specific steps to speed up your recovery in order to prevent injury. Depending on the duration of symptoms and the severity of the case, OTS is a serious condition which can take a long time to recover from. OTS not only affects the muscular system, but also the circulatory system, the nervous system, and the hormone regulation system. Recognizing the warning signs early and being proactive in prevention will help you to avoid OTS. If you’re already suffering, use the following tips and strategies in your recovery.
10 Tips to Self-Treat Overtraining Syndrome:
- Rest. One of the first and primary treatments for OTS is to rest. More rest is required the longer the overtraining has occurred. Therefore, early detection is critical. If the overtraining has only occurred for a short period of time (such as three to four weeks), then a brief three to five days of rest may be sufficient while implementing the following treatment strategies. After the rest days, slowly taper back into training at a lower training volume until recovery is complete. Typically, the intensity of training can be maintained as long as the volume is decreased. I also advise that you start an alternate day recovery cycle. Train for one day, and then take a day off. This will typically last for a few more weeks before resuming your normal training cycle. As you resume full training, it is important that the warning signs of overtraining are identified and corrected. In more severe cases, the training program may have to be interrupted for weeks or months for a full recovery.
- Cross train. Opt for an alternate form of exercise to help prevent exercise withdrawal syndrome. If you are heavily participating in CrossFit or running, choose leisurely cycling and yoga as part of your cross training routine. The key is to keep both training volume and intensity low while preserving a baseline of fitness. Most of the medical studies on overtraining are geared toward single sport athletes. For triathletes and other multi-sport athletes, the recovery process may be different depending on the circumstances. If you can identify that the overtraining has occurred in only one discipline, then resting from that discipline (as well as significantly decreasing training in the other sports) may result in a full recovery. Don’t try to substitute more workouts in one sport in order to compensate for rest in another. This will only worsen the symptoms of OTS, which affects both the parasympathetic (PSN) and sympathetic nervous system (SNS). Resting from overtraining on the bicycle by swimming more will help to rest fatigued quadriceps. However, stress is stress to the cardiovascular, nervous, and hormone systems. Cross training is an important component in your recovery. Incorporate it in your typical training cycles as a method to limit your risk of injury. Cross training can make training more enjoyable as it keeps your body stimulated and ready for improvement. As you recover from OTS, the volume and intensity must be significantly reduced to allow for adequate rest and recovery.
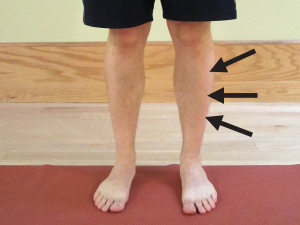
- Spot train your weak areas. In addition to cross training, use this recovery time to spot train your weak areas. Work on your mobility and balance as a prevention technique for areas that are prone to injury. If you have a history of low back pain or a prior knee injury, utilize this time to single out all those weak areas in an effort to prevent injury in the future. As you rest from your primary training routine while incorporating cross training, perform spot training as well. The Resource Guide includes a specific exercise section with rehabilitation exercises ranging from low back pain to knee pain. These .pdf files include photos and detailed descriptions to help you get started on spot training your weak areas. This is also an excellent time to work on the specific technical skills that your sport requires. It may include learning how to mentally manage your sport better.
- Actively manage your aches and pains. Consider seeing a masseuse for regular body work. Another option is to use the foam roller after exercise to speed up recovery times and decrease the risk of muscle soreness or restriction. To learn how to use a foam roller for self-treatment, please refer to Foam Rolling for Rehabilitation.
- Acupuncture. Incorporating acupuncture into your recovery process can be very beneficial. Acupuncture can help to address a multitude of conditions which affect the nervous, muscular, and hormonal systems. All three systems should be addressed during the recovery process. Along with many of my clients, I have experienced wonderful results with acupuncture. I highly recommend an acupuncturist who specializes in sports medicine and has experience treating athletes. During acupuncture sessions, you can take time to specifically work on intentional relaxation and meditation which has the added benefit of addressing the nervous and hormonal systems.
- Seek help early. If you are experiencing chronic aches or pain or are struggling with an aspect of your training, seek help immediately. A healthy lifestyle is a lifelong pursuit. If you are injured or not enjoying an activity, you will not stay engaged or motivated in the long term. Seeking advice specifically from an experienced coach, physical therapist, or physician can be beneficial.
- Decrease the stimulants. It is important to take steps to help both the nervous and hormonal system re-regulate and rejuvenate. Often with OTS, the adrenals become overtaxed and the level of cortisol (a stress hormone) is too high. Intake of stimulants, such as caffeine, tends to worsen the condition. Remember, caffeine can be found in many pre-work out supplements, running gels, soda, coffee, and tea as well as some over the counter (OTC) medications. During your recovery phase, limiting chemicals that promote stimulation to the nervous and hormonal systems (particularly in regard to cortisol and adrenal function) will speed up your recovery. Once you have recovered and are tapering back into full training, I caution you in limiting stimulants as a prevention strategy for future episodes of OTS.
- Eat healthy. A healthy diet is critical to avoid injury. Your body tissue needs nutrients to be able to perform at a high level. Avoid processed food as much as possible. Limit sugary food and add more protein and healthy fat in your diet. Maintaining a diet with adequate healthy fats is essential in providing the nutrients to support all hormone function in the body as well as support the brain and nervous system. In the case of OTS, I encourage that you consume a higher fat diet to help your body’s hormonal system re-regulate. Also, adequate protein intake is necessary to support muscle health and development. For more information on protein intake, please refer to How Much Protein Do I Really Need?
- Hydrate more frequently. The human body is primarily made of water, which is critical for all body functions. In the case of OTS, I highly encourage you to hydrate more frequently during recovery. Adequate water intake is critical to avoid dehydration which can negatively affect your training. Dehydrated tissues are prone to injury as they struggle to gain needed nutrients to heal and repair. Dehydrated tissues are less flexible and tend to accumulate waste products. Stay hydrated by drinking water. Try to avoid beverages that contain artificial sweeteners or chemicals with names you can’t spell or pronounce. Coconut water is a popular drink that offers vital nutrients. Also, consider a juicing cleanse with a heavy focus on the kidneys and liver to help detoxify the body.
- Supplement. My most recommended supplement to help recover from injury is CapraFlex by Mt. Capra. Essentially, it combines an organic glucosamine and chondroitin supplement with other natural herbs which are designed to reduce inflammation. CapraFlex can be taken long term or intermittently. In the case of OTS, I also recommend a colostrum supplement called CapraColostrum by Mt. Capra. Colostrum is the first milk produced by female mammals after giving birth. It contains a host of immunoglobulins, anti-microbial peptides, and other growth factors. It is especially good at strengthening the intestinal lining which prevents and heals conditions associated with a leaky gut. Colostrum can also help a person more effectively exercise in hotter conditions. Over all, it can boost the immune system, assist with intestinal issues, and help the body to recover faster. Like CapraFlex, Tissue Rejuvenator by Hammer Nutrition contains glucosamine and chondroitin as well as a host of herbs, spices, and enzymes to help support tissues and limit inflammation. I recommend taking either CapraFlex OR Tissue Rejuvenator. You can take CapraColostrum independently or in conjunction with either CapraFlex or Tissue Rejuvenator. I recommend taking these supplements as a recovery strategy. I recommend initially trying a 30 day protocol. If the supplements are aiding your recovery, you may choose to continue taking them for an additional 30 days. I implement this protocol as part of a prevention strategy during times of heavy volume or high intensity training. (Please consult with your pharmacist and/or physician prior to starting any new supplementation protocol. Herbs could interact with some medications particularly if you are taking blood thinners.)
Overtraining Syndrome can be dangerous and severely limit your ability to train. It also significantly increases your risk of injury. A recovery protocol should include a multifaceted approach that incorporates strategies to positively affect the muscular, nervous, and hormonal systems.
Nothing can derail your best laid training plans and goals like an injury or suffering from OTS! If you develop OTS, you will need to take specific steps to speed up your recovery in order to prevent injury and return to a normal training schedule.
AVAILABLE NOW ON AMAZON!
In my book, Preventing and Treating Overtraining Syndrome, I show you how to recognize the risk factors and symptoms of OTS. You’ll learn how to utilize prevention strategies to help you develop a personal training strategy that will allow you to push past your limits and prior plateau points in order to reach a state of what is known as overreaching (your body’s ability to “supercompensate”). This will speed up your results, so that you can train harder and more effectively than ever before! In addition, learn how to use the foam roller (complete with photos and detailed exercise descriptions) as part of a health optimization program, recovery program, rest day or treatment modality.
Discover how you can continue to train hard and avoid the associated poor performance, illness, and injury that can result in lost training days and opportunity!