Muscle pain is common and often occurs after exercise or activity. Although the pain is uncomfortable, most types of muscle pain are benign and quickly pass. Muscle aches and pains can affect your ability to compete or train at a high level. It also can affect your sleep and mood. Discover the possible causes of muscle pain as well as prevention and treatment strategies.
Possible Causes of Muscle Pain include:
- Delayed Onset Muscle Soreness (DOMS). This soreness typically occurs 24-48 hours after an exercise session due to micro trauma within the muscle tissue. It tends to be worse after eccentric biased exercise where the muscle is lengthened.
- Muscle Strain. If you strain your muscle either by over lengthening or over exerting the muscle capacity, muscle tearing may occur. Depending on the size and location of the tear, it may range from minor to severe (potentially needing surgical intervention).
- Myofascial Issues. Layers of the myofascia (the dense, tough tissue which surrounds and covers all of your muscles and bones) may become bunched or knotted up and result in pain. This is typically due to poor posture, repetitive motion injuries or over exertion.
- Neurological Issues. Many neurological disorders, including pinched nerves, can cause pain. Other medical conditions, such as muscular dystrophy, cause muscle dystonia.
- Illness. Muscle pain can occur as a symptom in colds, flu, Rocky Mountain Spotted Fever, and other viral or bacterial infections.
- Disease. Many diseases, such as Polio, Lupus, and Lyme’s Disease, cause muscle pain.
- Medications. Certain medications, such as statin drugs for cholesterol, have been strongly associated with muscle pain.
- Fibromyalgia. This condition causes muscle pain, joint pain, and extreme fatigue.
- Rhabdomyolysis. A serious condition, due to either direct or indirect muscle trauma, which causes pain. It can be life threating due to the potential for kidney failure. Common causes include extreme exercise, statin medication, severe injury or illicit drug use.
- Compartment Syndrome. A serious condition in which excessive swelling and pressure build up in a confined space. It leads to extreme muscle pain and eventually, numbness and tissue death.
This list highlights some of the many potential causes of muscle pain. Many are benign while others are true medical emergencies. The most common reasons include: delayed onset muscle soreness (DOMS); muscle strains; myofascial related issues due to posture and/or repetitive motion injuries; and fibromyalgia.
In order to properly treat muscle pain, first identify the cause of your muscle pain. Can you correlate the symptoms with a certain activity or exercise? Are you suffering from a cold or flu like symptoms? If you are unable to correlate a reason for the pain, then you may consider consulting with your medical physician to rule out other possible causes for muscle pain.

The following tips and strategies to treat muscle soreness specifically address mechanical causes related to DOMS, minor muscle strains, and myofascial issues. Many of these strategies are also appropriate in helping to manage fibromyalgia symptoms.
14 Tips and Strategies to Self-Treat Muscle Pain:
- Fix Your Posture. Poor posture is one of the most common causes of muscle spasming and pain. This is particularly true if you spend a good portion of your day sitting. Sign up to receive my weekly blog posts via e-mail, and I will share with you My Top 8 Stretches to Eliminate Neck, Upper Back, and Shoulder Pain. These simple exercises, with complete instructions and photos, will help you to improve poor posture and can be performed at home.
- Massage. Contact a masseuse, physical therapist, athletic trainer or friend who is skillful in body work and massage to relieve the area in spasm. The specific massage technique to use will vary according to your preference. Massage techniques range from a light relaxing massage to a deep tissue massage or utilization of acupressure points.
- Foam Roller. The foam roller allows you to perform self-massage and tissue mobilization. The foam roller is a wonderful tool to prevent muscle cramping and spasms. Please refer to the following posts for more information: Foam Rolling For Rehabilitation and 5 Ways to Improve Range-Of-Motion. I highly recommend a High Density Foam Roller to help aid in your recovery.
- Other Self-Mobilization Tools. Many times, a friend or masseuse isn’t available to assist when you need the help the most. A foam roller cannot effective reach places in the upper back or arms, so other self-mobilization tools may be necessary. You can get creative and use a tennis ball or golf ball, but I like a specific tool called a Thera Cane Massager. This tool allows you to apply direct pressure to a spasming muscle. When held for a long enough period of time, the Thera Cane Massager will usually cause the muscle spasms to release and provide much needed pain relief! I am also a big fan of the Thera-Band Standard Roller Massager. I particularly like that its firmness allows for a deep amount of pressure. If you prefer something similar, but more flexible for the boney regions of the thigh or lower leg, I recommend The Stick Self Roller Massager.
- Topical Agents. Many topical agents can help to decrease and eliminate muscle spasms. The method of action varies greatly according to the product used. You may find that one product works better than another. Some of my favorite products in my medicine cabinet include: Biofreeze Pain Relieving Gel; Arnica Rub (Arnica Montana, an herbal rub); and topical magnesium.
- Magnesium Bath. The combination of warm water with magnesium is very soothing and relaxing. Magnesium is known to help decrease muscle pain and soreness. Options include: Epsoak Epson Salt or Ancient Minerals Magnesium Bath Flakes. I find that the magnesium flakes work better, but they are significantly more expensive than Epson salt.
- Oral Magnesium. You can take Mag Glycinate in pill form or by eating foods higher in magnesium such as spinach, artichokes, and dates. Taking additional magnesium (particularly at night) can help to reduce muscle cramps and spasming. It is also very helpful in reducing overall muscle soreness and aiding in a better night’s rest. Most people are deficient in the amount of magnesium they consume on a regular basis. I recommend beginning with a dose of 200 mg (before bedtime) and increasing the dose as needed. I would caution you that taking too much magnesium can lead to diarrhea. Mag Glycinate in its oral form is the most highly absorbable. Although not as absorbable, Thorne Research Magnesium Citrate and magnesium oxide can also be beneficial.
- Stay Hydrated. The human body is primarily made of water, which is critical for all body functions. Your muscles are approximately 80% water. Dehydrated tissues are prone to injury and pain as they struggle to gain needed nutrients to heal and repair. Dehydrated tissues are less flexible and tend to accumulate waste products. Stay hydrated by drinking water. Try to avoid beverages that contain artificial sweeteners or chemicals with names you can’t spell or pronounce.
- Eat Healthy. A healthy diet is critical to avoid injury, illness, and pain. Your body tissue needs nutrients to be able to perform at a high level. Avoid processed food as much as possible. Limit sugary food and add more protein and healthy fat in your diet. Maintaining a diet with adequate healthy fats is essential in providing the nutrients to support all hormone function in the body as well as support the brain and nervous system. Adequate protein intake is necessary to support muscle health and development. Give your body the needed nutrients to combat illness and function at a high level.
- Move More! Not only has research proven that sitting for more than two hours at a time decreases your expected life span, but extended sitting also leads to increased muscle tension, cramping, and pain. If you sit most of the day, get up and walk. If you stand most of the day, frequently change your standing posture. To optimize health and joint function, you should take each joint in your body through a least one full range of motion (ROM) every day. If you are experiencing pain, I recommend performing more frequent ROM (every 1-2 hours).
- Stretch. Stretching is a wonderful way to help eliminate a muscle spasm. We instinctively stretch when we feel a spasm begin. Try gently stretching (lengthening) the muscle affected by the spasm. I recommend beginning with a short 30-60 seconds stretch, then repeating as needed. If the spasm or cramp is severe, you will likely need to continue stretching several times in a row, multiple times throughout the day. Stretching should always be part of a general fitness and lifestyle program. As we age, muscle and tendons tend to lose elasticity so stretching becomes even more important. I highly recommend a daily stretching routine or participation in a group class, such as yoga, which incorporates full body stretching.
- Acupuncture. I am personally a big fan of acupuncture. It is very useful in treating all kinds of medical conditions. It can be particularly effective in treating muscle cramps, spasms, and pain as it addresses the issues on multiple layers. Acupuncture directly stimulates the muscle by affecting the nervous system response to the muscle while producing a general sense of well-being and relaxation.
- Sleep and Rest More. Most people are not sleeping long enough or often enough to optimize health. Take a nap or go to bed earlier. Your body requires time to repair and heal as you sleep. Your body must rest in order to grow and develop. Training every day is not the best way to improve. It can lead to injury and burn out. Take a rest day and have fun. Participate in a Tai Chi or yoga class, take a leisurely bike ride or take a walk in the park.
- Speak with your Physical Therapist (PT) or Physician (MD). If your muscle pain cannot be correlated to a specific mechanical cause, please speak to your medical provider to determine if other causes are contributing to the problem. The American Physical Therapy Association (APTA) offers a wonderful resource to help find a physical therapist in your area. In most states, you can seek physical therapy advice without a medical doctor’s referral (although it may be a good idea to hear your physician’s opinion as well).
Most muscle pain and soreness can be self-managed and self-treated if you are proactive. These tips and strategies are highly effective in managing muscle pain. A healthy lifestyle is a lifelong pursuit. If you are injured or not enjoying an activity, you will not stay engaged or motivated in the long term. Seeking advice specifically from a running coach, physical therapist or physician can be beneficial.
How do you manage your aches and pains? Which tip or strategy will you incorporate into your treatment? Please leave your comments below.
If you have a question that you would like featured in an upcoming blog post, please comment below or submit your question to contact@thePhysicalTherapyAdvisor.com. Be sure to join our growing community on Facebook by liking The Physical Therapy Advisor!
Disclaimer: The Physical Therapy Advisor blog is for general informational purposes only and does not constitute the practice of medicine or other professional health care services, including the giving of medical advice. No health care provider/patient relationship is formed. The use of information on this blog or materials linked from this blog is at your own risk. The content of this blog is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Do not disregard, or delay in obtaining, medical advice for any medical condition you may have. Please seek the assistance of your health care professionals for any such conditions.
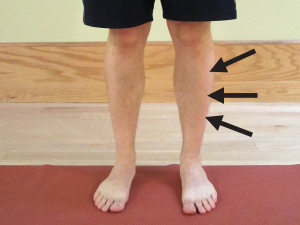 The term shin splints, also known as an anterior compartment syndrome, refers to pain along the shinbone (tibia), the large bone in the front of your lower leg. Shin splints can be excruciatingly painful to the point that you may struggle to walk or run. They are typically caused by inflammation in the anterior muscle of the lower leg known as the anterior tibialis muscle. This is the primary muscle needed to lift your foot. Shin splints are often considered an over use injury and unfortunately, are relatively common in runners. Discover the common causes for shin splints and implement these strategies to prevent and self-treat shin splints. Continue Reading
The term shin splints, also known as an anterior compartment syndrome, refers to pain along the shinbone (tibia), the large bone in the front of your lower leg. Shin splints can be excruciatingly painful to the point that you may struggle to walk or run. They are typically caused by inflammation in the anterior muscle of the lower leg known as the anterior tibialis muscle. This is the primary muscle needed to lift your foot. Shin splints are often considered an over use injury and unfortunately, are relatively common in runners. Discover the common causes for shin splints and implement these strategies to prevent and self-treat shin splints. Continue Reading