Q. I fell snowboarding last weekend, and I broke my collarbone. My doctor says that I don’t need surgery and that I will be fine in a couple of months. I want to be more proactive than that. What should I do? -Shawn
A. Thanks for the question, Shawn. I’m sorry to hear about your snowboarding accident. Fractures of the collarbone (clavicle) are actually fairly common and typically result from falling on the shoulder, the collarbone or an outstretched hand. Collarbone injuries are also very common in toddlers, typically due to a fall out of bed or tripping when running.
The collarbone attaches the sternum to the scapula (shoulder blade). Many important structures, such as nerves and blood vessels, lie just below the clavicle. However, these vital structures are rarely injured when the clavicle breaks. Diagnosing a clavicle fracture is typically performed via X-ray. In certain circumstances, a CT Scan may be performed for a more thorough image of the injury.

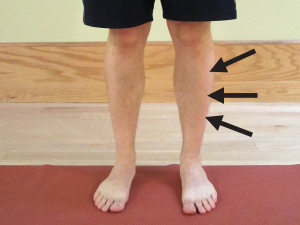
Symptoms of a Collarbone Fracture include:
- Pain in the shoulder or over the collarbone.
- Difficulty raising your arm due to pain.
- Slumping or sagging of the shoulder, typically downward and forward.
- A grinding sensation in the collarbone area when attempting to raise the arm.
- A “bump” forms over the collarbone. In severe cases, the bump will be similar to a piano key sticking up and will be mobile.
- Bruising and swelling over the collarbone area.
Surgical Intervention
Depending on the severity of the injury, surgery may or may not be indicated. In most cases, a simple fracture (where the bones are still aligned) will not require surgery. Even in cases of minor malalignment, most people will not undergo surgery.
Surgical fixation is most common when there is a significant displacement or malalignment present. The purpose of surgical fixation is to hold the bones in place while they heal. The physician will either utilize a metal plate and screws or small pins to hold the bones in place. Although the surgical hardware can be removed once the bones have sufficiently healed, often it will remain throughout a person’s lifetime.
Rehabilitation post-surgery is fairly straight forward and is similar to the following nonsurgical treatment recommendations. Please follow your physician’s recommendations after surgery as each procedure can be different. Variations in recovery and rehabilitation can occur and are dependent on: the area that was fixed; the severity of the fracture; and the stability of the bone and fixation. These factors will determine how quickly you can progress through the rehabilitation.
Nonsurgical Treatment Recommendations
Most collarbone fractures do not require surgery (particularly, if the fractured area retains its alignment). Your physician will assess the severity of the fracture. This will determine how quickly you can progress through the stages of treatment.
A general time frame for healing (with an initial return to function) is on average 6 weeks for adults and about 4 weeks for children. Complete bone healing, remodeling, and a full return to all activities will take longer. This will depend on your age, health status, and the severity of the injury.
PRICE (Protect, Rest, Ice, Compression, and Elevation)
- Protect. In many cases, you will be advised to wear a sling (particularly, during your daily activities). This will help to protect the area from too much motion and activity while allowing the bone to heal in its proper place. It will also indicate to others that you have an injury, so that they may avoid knocking into you.
- Rest. Allow the arm and shoulder time to rest and recover. Do not utilize the arm for activities that cause pain. Avoid excessive motions and use. As the pain subsides, you can slowly taper up the use of the arm by starting with simple daily activities.
- Ice. Apply ice to the painful area–typically the sooner, the better. The rule for icing is to apply ice no more than twenty minutes per hour. Do not place the ice directly against the skin, especially if you are using a gel pack style. A bag of frozen peas can be ideal. Individuals with poor circulation or impaired sensation should take particular care when icing.
- Compression. It’s not easy to apply compression in this area. In most cases, it’s not necessary. In some cases, a simple ACE wrap can be used around the shoulder and collarbone area to help reduce the pain. The wrap is typically applied to help hold the shoulder in a backward and slightly downward direction.
- Elevation. Elevation is typically not necessary unless you are experiencing excessive swelling in the affected arm and hand. You can position the arm in a slightly elevated position by using pillows while lying on your back or on the non-affected side. This would be an excellent time to apply ice, too.
Sleeping
When sleeping, try not to lie on the affected side. Hug a small pillow for comfort. This also promotes optimal blood flow to the shoulder area.
Pain Management
Initially begin with PRICE (Protect, Rest, Ice, Compression, and Elevation). Pain medication, such as acetaminophen, is always an option if recommended by your physician. You may also want to consider utilizing topical agents, which can help to decrease pain and muscle spasms. The method of action varies greatly according to the product used. You may find that one product works better than another. Some of my favorite products in my medicine cabinet include: Biofreeze Pain Relieving Gel; Arnica Rub (Arnica Montana, an herbal rub); and topical magnesium.
Another option is oral magnesium. You can take Mag Glycinate in pill form or by eating foods higher in magnesium such as spinach, artichokes, and dates. Taking additional magnesium (particularly at night) can help to reduce muscle cramps and spasming. It is also very helpful in reducing overall muscle soreness and aiding in a better night’s rest. Most people are deficient in the amount of magnesium they consume on a regular basis. I recommend beginning with a dose of 200 mg (before bedtime) and increasing the dose as needed. I would caution you that taking too much magnesium can lead to diarrhea. Mag Glycinate in its oral form is the most highly absorbable. Although not as absorbable, Thorne Research Magnesium Citrate and magnesium oxide can also be beneficial.
Supplements
Mt. Capra, an organic goat farm in eastern Washington State, offers superior quality products primarily utilizing goat based products. CapraFlex by Mt. Capra is the best bone and joint supplement I have found. It is a blend of natural herbs and spices along with glucosamine and chondroitin. The herbal and spice formulation is designed to naturally decrease inflammation and support healing. I recommend it to anyone recovering from an injury or attempting to prevent injury when performing at a very high level. I personally use it, and in my practice, it has helped clients recover faster and prevent injury. It can interfere with some blood thinning medication, so if you are on this type of medication, please check with your physician.
Vitamin D3, such as Viva Labs Vitamin D3, is critical to the absorption of calcium through the intestinal wall which is important for bone health. Although calcium is a critical component of bone health, I cannot recommend extra supplementation because of the potential cardiac risks to over supplementation. A healthy varied diet will typically supply adequate calcium levels (assuming that adequate Vitamin D3 levels are present for absorption and that you are avoiding drinking soda). Vitamin D3 is also a critical nutrient in maintaining a healthy immune system.
Be sure to maintain a generally healthy diet. Give your body the needed nutrients to heal and recover quickly.
Range of Motion
Depending on the severity of the fracture, you will likely have to limit the range of motion (ROM) of the shoulder to less than 70-80 degrees of flexion (forward) and abduction (sideways) motion. You will also have to limit reaching behind your back. A person may typically wear a sling for 2-4 weeks while limiting the motion.
The initial treatment to maintain ROM is to perform the pendulum exercise (as demonstrated in the picture on the left down below). Bend forward at the waist, and let your injured arm hang down toward the ground. Make small circles with your hand, and let the momentum move your arm around effortlessly. Try to make both clockwise and counterclockwise circles. For more instruction, please watch How to Properly Perform Pendulum Exercises.

Around the 2-4 weeks mark, you can begin to work on regaining full forward flexion by using an over-the-door shoulder pulley (as demonstrated in the picture on the above right). Work slowly on motion for 5-10 minutes at a time. You may push though minor discomfort, but you should never experience significant pain during this process. For more instruction, please watch How to Use Shoulder Pulleys to Regain Shoulder Motion.
As flexion improves (typically after the 4 weeks mark), then you can begin to work on all other motions of the shoulder. This includes motion out to your side (abduction) and behind your back (internal rotation). The shoulder pulley can be utilized to regain these motions as well. Otherwise, you could walk your fingers up the wall when facing forward to regain flexion and sideways to regain abduction. You could use a towel to regain the motion behind your back.
Strengthening
Initially avoid lifting anything over 5 pounds. Typically around the 4-6 weeks mark (depending on severity of injury), you can begin a gentle rotator cuff strengthening program. These exercises should always be performed pain free and initially, the resistance will be very light. For specific exercises, please refer to Rotator Cuff Exercises.
The rotator cuff is a critical component to shoulder mobility. It is made up of four different muscles whose job is to make sure that the ball of the humerus (arm bone) rotates and slides properly in the socket, which is made up of the scapula. The rotator cuff allows the other major muscles of the arm, such as the deltoid and Latissimus dorsi (lats), to properly move the arm.
When there is weakness or dysfunction, it will cause rubbing of the muscle tendon on the bone. This can lead to impingement or eventually fraying and tearing. Insuring proper strength in the rotator cuff after a collarbone injury is an important component in avoiding shoulder impingement syndrome.
Return to Full Activity
Around the 8-12 weeks mark, you will likely consult with your physician to have another X-ray taken. Once you’re cleared by your physician, you can slowly taper back into more strenuous exercises and a return to full activity.
If your injury was severe or required surgery, it may be closer to the 16 weeks mark before you can return to full activity and be cleared to lift heavier weights. I recommend that you slowly taper back into your prior activities. If you are experiencing pain, then back off that particular activity and try it again at a later date.
Help from a Physical Therapist (PT)
Every injury is different. If you’re experiencing pain or difficulty regaining your strength and shoulder range of motion, please consult with a physical therapist that is an orthopaedic certified specialist (OCS). The American Physical Therapy Association (APTA) offers a wonderful resource to help find a physical therapist in your area. In most states, you can seek physical therapy advice without a medical doctor’s referral (although it may be a good idea to hear your physician’s opinion as well).
Good luck, Shawn! I hope you find this information to be helpful and provide some relief from the pain you’re experiencing.
Have you broken your collarbone? What was your experience like? Please share your best tips for recovery.
If you have a question that you would like featured in an upcoming blog post, please email contact@thephysicaltherapyadvisor.com. For additional health and lifestyle information, join our growing community on Facebook by liking The Physical Therapy Advisor!
Disclaimer: The Physical Therapy Advisor blog is for general informational purposes only and does not constitute the practice of medicine or other professional health care services, including the giving of medical advice. No health care provider/patient relationship is formed. The use of information on this blog or materials linked from this blog is at your own risk. The content of this blog is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Do not disregard, or delay in obtaining, medical advice for any medical condition you may have. Please seek the assistance of your health care professionals for any such conditions.
 Metatarsalgia is a general term that refers to pain in the foot (typically around the ball of the foot). It’s common in runners, track and field athletes, and for those who participate in high impact related sports (such as basketball and soccer). It’s also commonly associated with overuse syndrome.
Metatarsalgia is a general term that refers to pain in the foot (typically around the ball of the foot). It’s common in runners, track and field athletes, and for those who participate in high impact related sports (such as basketball and soccer). It’s also commonly associated with overuse syndrome.