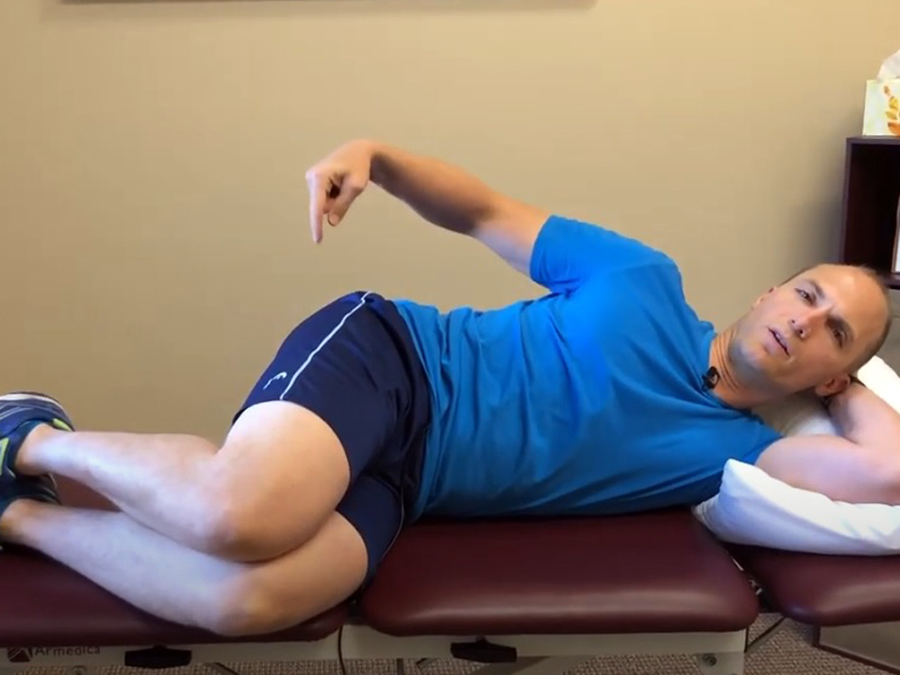
Weakness in the deep external rotation muscles and poor lower extremity single leg balance are commonly associated with many lower extremity overuse injuries. A simple and effective exercise to improve strength, balance, and general stability of the deep hip external rotator muscles is the clock exercise (also called the star drill).

The important points to remember in this exercise are to keep the stance knee unlocked (the leg you are standing on) with the patella (knee cap) slightly externally rotated (usually pointing towards the 3rd or 4th toe). The rotation must come from the hip, NOT the ankle. The stability of the hip and activation of the deep hip external rotators needs to be the primary focus.
Slowly touch the ground very gently with the opposite leg. The amount of pressure touching the ground should be so slight that if there were a package of crackers taped to the bottom of the foot the crackers would not break. Performing the drill on a balance pad will significantly increase the difficulty level of the exercise.
In the following video, I demonstrate how to use a balance pad to perform the clock exercise, a key lower leg stability exercise for treating knee pain, hip pain, and foot and ankle related issues as well as balance.
For additional videos on my recommended exercises to increase hip strength and stability, be sure to check out:
- Standing Hip 3-Way Exercise
- How to Use the Clamshell Hip Exercise to Treat Knee Pain
- The Clock Exercise for Knee and Hip Pain and Stability
For prevention strategies and to learn more about on how to self-treat the most common lower extremity overuse injuries, be sure to check out the Resilient Runner Program, which is designed to help YOU meet YOUR training goals by insuring you have the tools to avoid injury, recover quickly, and train at a peak level.
Have you performed the clock exercise before? If so, what was your experience like? Please leave your comments below.
If you have a question that you would like featured in an upcoming blog post, please comment below or submit your question to contact@thePhysicalTherapyAdvisor.com. In case you haven’t already, be sure to subscribe to my e-mail list and YouTube channel as well as join our community on Facebook by liking The Physical Therapy Advisor!